Prostate Cancer Questions & Answers
Below are the answers to the most asked question on prostate cancer.
PROST! is a prostate cancer support group to provide assist men and their families through the prostate journey. We provide this information to assist in the journey.
What is prostate cancer?
Prostate cancer is a type of cancer that occurs in the prostate, a small walnut-shaped gland located just below the bladder in men. The prostate gland produces seminal fluid, which nourishes and transports sperm. Prostate cancer develops when the cells in the prostate gland begin to grow uncontrollably.
The exact cause of prostate cancer is unknown, but certain risk factors have been identified. These include age (prostate cancer is more common in older men), family history of prostate cancer, race (Australian aboriginal men have a higher risk), and certain genetic changes.
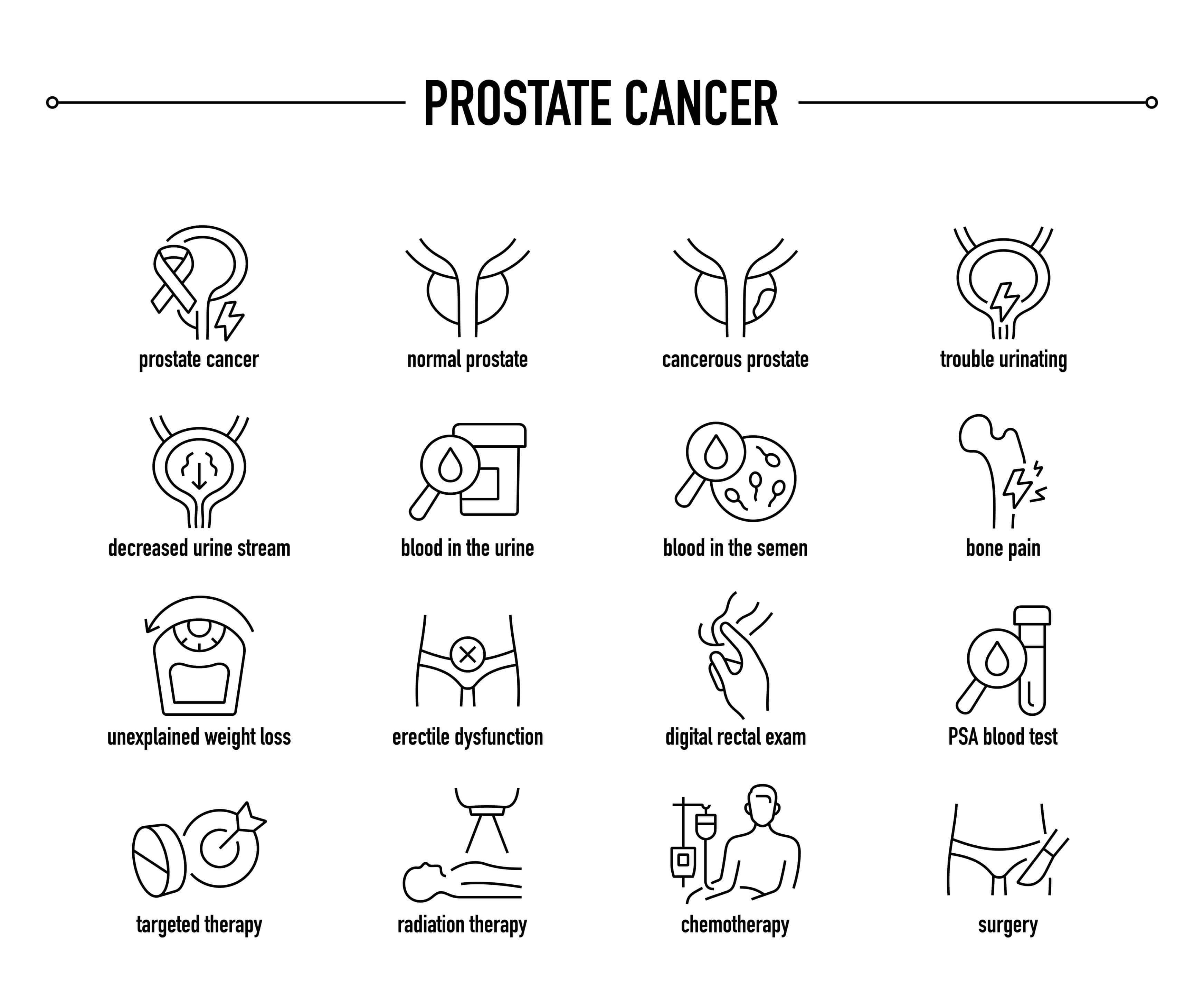
In the early stages, prostate cancer may not cause any noticeable symptoms. However, as the disease progresses, symptoms may include difficulty urinating, weak urine flow, blood in the urine or semen, erectile dysfunction, pain in the hips, back, or pelvis, and bone pain.
Prostate cancer is typically diagnosed through a combination of a digital rectal examination (DRE), a blood test called prostate-specific antigen (PSA) test, and a prostate biopsy. Once diagnosed, the cancer is assigned a stage based on its size, location, and spread.
Treatment options for prostate cancer depend on various factors, including the stage of the cancer, the aggressiveness of the tumour, the overall health of the patient, and their personal preferences. Treatment options may include active surveillance (regular monitoring without immediate treatment), surgery, radiation therapy, hormone therapy, chemotherapy, immunotherapy, or a combination of these approaches.
It's important for men to discuss prostate cancer screening and risk factors with their healthcare providers, especially if they are at an increased risk. Early detection and appropriate treatment can significantly improve the outcomes for individuals with prostate cancer.
What are the risk factors for prostate cancer?
Several risk factors have been identified for prostate cancer. These factors may increase a man's likelihood of developing the disease. Here are some of the key risk factors:
a) Age: Prostate cancer is more common in older men. The risk increases significantly after the age of 50, and the majority of cases are diagnosed in men over 65.
b) Family history: Having a close relative, such as a father or brother, with prostate cancer increases the risk. The risk is even higher if the relative was diagnosed at a young age or if multiple family members are affected.
c) Race and ethnicity: Prostate cancer is more prevalent among Australian aboriginal men than men of other racial or ethnic backgrounds. It tends to be more aggressive and diagnosed at more advanced stages in this population.
d) Genetics: Certain inherited gene mutations, such as mutations in the BRCA1 and BRCA2 genes, are associated with an increased risk of prostate cancer. These mutations are also linked to an increased risk of other cancers, such as breast and ovarian cancer.
e) Lifestyle factors: Several lifestyle factors may contribute to the risk of developing prostate cancer. These include a diet high in red meat and dairy products, obesity, smoking, and lack of physical activity. However, more research is needed to fully understand the impact of these factors on prostate cancer risk.
It's important to note that having one or more risk factors doesn't necessarily mean that a person will develop prostate cancer. Likewise, some individuals without any identifiable risk factors may still develop the disease. Regular screenings and discussions with a healthcare provider are crucial for early detection and appropriate management of prostate cancer.
What are the symptoms of prostate cancer?
In the early stages, prostate cancer may not cause any noticeable symptoms. However, as the disease progresses, symptoms may start to manifest. It's important to note that these symptoms can also be caused by non-cancerous conditions, but if you experience any of the following, it's advisable to consult with a healthcare professional for further evaluation:
a) Urinary symptoms: Changes in urination are common in prostate cancer. These may include:
Frequent urination, especially at night (nocturia)
Difficulty starting or stopping urination
Weak urine flow or interrupted flow
Urgency to urinate
Inability to empty the bladder completely
b) Blood in urine or semen: Prostate cancer can cause blood to appear in the urine (hematuria) or semen (hematospermia). If you notice blood in either of these fluids, it's essential to seek medical attention.
c) Erectile dysfunction: Prostate cancer can affect sexual function. Difficulties achieving or maintaining an erection (erectile dysfunction) may occur.
d) Pain or discomfort: As prostate cancer progresses, it can cause pain or discomfort in various areas, including:
Pelvic region, including the lower back, hips, or groin
Bones, which can lead to bone pain, particularly in the spine, hips, or ribs
It's important to remember that these symptoms can also be associated with other non-cancerous conditions such as benign prostatic hyperplasia (BPH) or prostatitis. However, if you experience any persistent or bothersome symptoms, it's advisable to consult a healthcare professional for further evaluation and appropriate testing, including a prostate-specific antigen (PSA) blood test and a digital rectal examination (DRE) if necessary. Early detection and timely treatment can significantly improve outcomes for prostate cancer.
How is prostate cancer diagnosed?
Prostate cancer can be diagnosed through several methods. Here are the primary approaches used for diagnosing prostate cancer:
a) Prostate-Specific Antigen (PSA) Test: The PSA test measures the level of prostate-specific antigen in the blood. Elevated PSA levels can indicate the presence of prostate cancer, although other factors like age, prostate size, and inflammation can also affect PSA levels. If the PSA test results are abnormal, further investigation is typically required.
b) Digital Rectal Exam (DRE): During a DRE, a healthcare provider inserts a gloved, lubricated finger into the rectum to feel the prostate gland. They assess the size, shape, and any abnormalities of the prostate. Although it cannot definitively diagnose prostate cancer, it helps detect irregularities that may require further evaluation.
c) Prostate Biopsy: A prostate biopsy is often performed if abnormalities are found during a PSA test or DRE. It involves the removal of small tissue samples from the prostate gland, typically guided by transrectal ultrasound (TRUS). The collected tissue samples are then examined under a microscope to determine if cancer is present, and if so, to assess the Gleason score for grading.
d) Imaging Tests: Imaging tests such as magnetic resonance imaging (MRI), computed tomography (CT) scans, or bone scans may be performed to evaluate the extent of the cancer, detect any spread to nearby tissues or distant organs, and determine the stage of prostate cancer.
It's important to note that the definitive diagnosis of prostate cancer is made through a prostate biopsy (Refer to Gleason Score). The combination of PSA testing, DRE, and biopsy results, along with other clinical information, helps healthcare professionals make an accurate diagnosis and determine the appropriate treatment plan for an individual with suspected prostate cancer.
What are the different stages of prostate cancer?
Prostate cancer staging is a way to describe the extent and spread of the disease. The most commonly used staging system for prostate cancer is the TNM system, which stands for Tumour, Node, and Metastasis. Here are the stages of prostate cancer according to this system:
a) Stage I: The cancer is confined to the prostate gland and is too small to be felt during a digital rectal examination (DRE) or seen on imaging tests. It may be detected incidentally during surgery for another prostate-related condition or may be found in a biopsy performed due to elevated prostate-specific antigen (PSA) levels.
b) Stage II: The cancer is still confined to the prostate gland but is larger and may be felt during a DRE. It may be detected through a biopsy or imaging tests. Stage II is further divided into two subcategories:
Stage IIA: The cancer is still confined to one-half or less of one side of the prostate gland.
Stage IIB: The cancer has spread to more than one-half of one side of the prostate gland.
c) Stage III: The cancer has spread beyond the prostate gland but is still localised in the nearby tissues. This stage may involve the seminal vesicles (small glands that produce semen) or other nearby structures.
d) Stage IV: The cancer has spread beyond the prostate and nearby tissues. It may involve nearby lymph nodes, bones, or other organs such as the bladder or rectum. Stage IV is further divided into two subcategories:
Stage IVA: The cancer has spread to nearby lymph nodes.
Stage IVB: The cancer has metastasized to distant sites, such as bones, liver, lungs, or other organs.
In addition to the TNM system, prostate cancer is also commonly categorised into low-risk, intermediate-risk, and high-risk groups based on various factors such as PSA levels, Gleason score (a measure of cancer aggressiveness), and clinical stage.
It's important to note that the specific staging and treatment decisions are best made in consultation with a healthcare professional who will consider various factors, including the results of imaging tests, biopsies, and other diagnostic procedures.
What treatment options are available for prostate cancer?
There are several treatment options available for prostate cancer, and the choice of treatment depends on various factors such as the stage of cancer, overall health of the patient, and patient preferences. Here are some common treatment options:
a) Active Surveillance: For slow-growing and early-stage prostate cancer, active surveillance may be recommended. This approach involves regular monitoring of the cancer through PSA (prostate-specific antigen) blood tests, digital rectal exams, and periodic biopsies. Treatment is deferred unless there are signs of cancer progression.
b) Surgery: Surgical removal of the prostate gland, known as radical prostatectomy, is a common treatment for localized prostate cancer. It can be performed using open surgery or minimally invasive techniques such as laparoscopic or robotic-assisted surgery. The entire prostate gland and sometimes nearby lymph nodes are removed.
c) Radiation Therapy: Radiation therapy uses high-energy X-rays or other types of radiation to kill cancer cells or prevent their growth. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy). Radiation therapy may be used as the primary treatment for localised prostate cancer or in combination with other treatments.
d) Hormone Therapy: Prostate cancer cells rely on male hormones, particularly testosterone, to grow. Hormone therapy, also called androgen deprivation therapy (ADT), aims to reduce the levels of male hormones or block their effects. This can be achieved through medications that suppress hormone production in the testicles or block their action in the body. Hormone therapy is often used in advanced or metastatic prostate cancer and may be combined with other treatments.
e) Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop their growth. It is typically used in advanced prostate cancer that has spread to other parts of the body. Chemotherapy may also be used in combination with hormone therapy for certain cases.
f) Immunotherapy: Immunotherapy is a relatively new treatment option for advanced prostate cancer. It works by stimulating the body's immune system to recognize and attack cancer cells. Immune checkpoint inhibitors, such as pembrolizumab or sipuleucel-T, are examples of immunotherapy drugs used in prostate cancer treatment.
g) Targeted Therapy: Targeted therapy uses drugs that specifically target certain genetic mutations or proteins present in cancer cells. In prostate cancer, targeted therapies like enzalutamide or abiraterone acetate may be used in advanced cases.
The choice of treatment and the combination of therapies will depend on the individual patient's case, and it's important for patients to discuss their options with their healthcare team to make an informed decision.
What are the potential side effects of prostate cancer treatment?
Prostate cancer treatment can have several potential side effects, which can vary depending on the specific treatment methods used. Here are some common side effects associated with different prostate cancer treatments:
a) Surgery:
Erectile dysfunction: Difficulty achieving or maintaining an erection.
Urinary incontinence: Inability to control urine flow or leakage.
Decreased semen volume: The amount of semen released during ejaculation may decrease.
Short-term pain and swelling: Temporary discomfort and swelling in the surgical area.
b) Radiation therapy:
Fatigue: Feeling tired or lacking energy.
Skin changes: Redness, irritation, or dryness in the treated area.
Urinary problems: Increased frequency of urination, urgency, or discomfort.
Bowel problems: Diarrhea, rectal irritation, or in rare cases, rectal bleeding.
Erectile dysfunction: May occur, but it is usually less common than with surgery.
c) Hormone therapy:
Erectile dysfunction: Difficulty achieving or maintaining an erection.
Hot flashes: Sudden feelings of warmth, often accompanied by sweating.
Loss of libido: Decreased sexual desire.
Breast enlargement or tenderness: Some hormonal treatments can cause breast tissue changes.
Osteoporosis: Weakening of the bones, leading to an increased risk of fractures.
d) Chemotherapy:
Fatigue: Feeling tired or lacking energy.
Nausea and vomiting: Possible temporary side effects during treatment.
Hair loss: Some chemotherapy drugs may cause hair loss, but it usually grows back after treatment.
Decreased blood cell counts: Chemotherapy can affect the production of red and white blood cells and platelets, leading to an increased risk of infection, anemia, or bleeding.
It's important to note that not everyone will experience these side effects, and their severity can vary from person to person. It's essential to discuss potential side effects with your healthcare team so that they can provide personalized guidance and support throughout your treatment journey.
How effective is treatment for prostate cancer?
The effectiveness of treatment for prostate cancer can vary depending on several factors, including the stage of cancer at diagnosis, the aggressiveness of the tumour, the overall health of the patient, and the specific treatment approaches used. Generally, treatment for prostate cancer can be quite effective, especially when the cancer is diagnosed at an early stage.
Here are some common treatment options for prostate cancer:
a) Surgery: Surgical removal of the prostate gland, known as a prostatectomy, can be a curative treatment for localised prostate cancer. The success of the surgery depends on the stage and extent of cancer and the surgeon's skill.
b) Radiation therapy: This treatment uses high-energy rays to kill cancer cells. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy). Radiation therapy is often used as a primary treatment for localised prostate cancer or as an adjuvant treatment after surgery.
c) Hormone therapy: Prostate cancer cells often rely on male hormones, particularly testosterone, for growth. Hormone therapy aims to block the production or action of these hormones, slowing down or shrinking the tumour. It is commonly used in advanced or metastatic prostate cancer and as an adjuvant treatment for high-risk localised disease.
d) Chemotherapy: Chemotherapy drugs are used to kill cancer cells or slow down their growth. Chemotherapy is typically used in advanced or metastatic prostate cancer when hormone therapy is no longer effective. It can also be used before surgery or radiation to shrink the tumour.
e) Targeted therapy: Targeted therapy drugs work by targeting specific genetic or molecular changes in cancer cells. They can block signals that promote cancer growth or stimulate the immune system to attack cancer cells. Some targeted therapies are approved for advanced prostate cancer, especially for patients with specific genetic mutations.
The effectiveness of these treatments varies depending on the individual case. For localised prostate cancer, the overall five-year survival rate is close to 100%. However, for advanced or metastatic prostate cancer, the prognosis is more variable, with the five-year survival rate ranging from around 30% to 90%, depending on the extent of the disease and the response to treatment.
It's important to note that each person's case is unique, and the effectiveness of treatment can vary. It's essential for patients to consult with their healthcare team to discuss the best treatment options based on their specific situation.
Are there any alternative or complementary treatments for prostate cancer?
Yes, there are several alternative or complementary treatments that are sometimes used alongside conventional medical treatments for prostate cancer. It's important to note that while these approaches may have some benefits, they are not intended to replace standard treatments, and their effectiveness may vary from person to person. It's always advisable to consult with a healthcare professional before pursuing any alternative or complementary treatments. Here are a few examples:
a) Herbal Supplements: Some herbal supplements, such as saw palmetto, pomegranate extract, green tea, and lycopene, have been studied for their potential benefits in prostate cancer. However, the evidence for their effectiveness is limited, and their use should be discussed with a healthcare provider.
b) Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body. It is often used for managing cancer-related symptoms, such as pain, nausea, and fatigue. While acupuncture may provide some relief, it should be used as a complementary therapy and not as a primary treatment for prostate cancer.
c) Dietary Changes: A healthy diet is important for overall well-being, including cancer prevention and management. Some dietary changes that may be beneficial include increasing the consumption of fruits, vegetables, whole grains, and lean proteins, while reducing the intake of processed foods, red meat, and saturated fats. It's worth noting that no specific diet has been proven to cure prostate cancer, but a balanced and nutritious diet can support overall health.
d) Mind-Body Techniques: Techniques such as meditation, yoga, and relaxation exercises can help reduce stress, anxiety, and improve overall well-being. These practices may complement medical treatments by promoting relaxation, improving sleep, and reducing the side effects of cancer treatments.
e) Exercise: Regular physical activity has been shown to have numerous health benefits, including reducing the risk of certain cancers and improving treatment outcomes. Exercise can help maintain a healthy weight, boost the immune system, reduce fatigue, and improve overall quality of life. However, it's important to consult with a healthcare professional before starting or modifying an exercise regimen.
It's crucial to emphasise that alternative or complementary treatments should not be used as a substitute for conventional medical care. They should be used in conjunction with standard treatments and under the guidance of a healthcare provider.

Can prostate cancer be prevented?
Prostate cancer prevention strategies aim to reduce the risk of developing the disease. While it is not possible to completely prevent prostate cancer, there are certain steps that may help reduce the risk or delay its onset. Here are some measures that have been suggested:
a) Healthy diet: Adopting a nutritious diet that includes a variety of fruits, vegetables, whole grains, and lean proteins may be beneficial. Some studies suggest that a diet rich in fruits and vegetables, particularly tomatoes and cruciferous vegetables like broccoli, may have a protective effect against prostate cancer. Additionally, limiting the consumption of processed meats and saturated fats may be helpful.
b) Regular exercise: Engaging in regular physical activity has been associated with a lower risk of prostate cancer. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week.
c) Maintain a healthy weight: Obesity and excess body weight have been linked to an increased risk of developing aggressive forms of prostate cancer. Therefore, maintaining a healthy weight through a balanced diet and regular exercise may be beneficial.
d) Quit smoking: Smoking has been linked to an increased risk of developing aggressive forms of prostate cancer. Quitting smoking not only reduces the risk of prostate cancer but also has numerous other health benefits.
e) Regular screening: While screening tests like the prostate-specific antigen (PSA) blood test are not considered preventive measures, they can help detect prostate cancer at an early stage when treatment is more effective. It is advisable to discuss the pros and cons of screening with your healthcare provider to make an informed decision.
It is important to note that these preventive measures may help reduce the risk of developing prostate cancer but cannot guarantee complete prevention. If you have concerns about prostate cancer or any other health condition, it is always best to consult with a healthcare professional who can provide personalized advice based on your individual circumstances.
What is the prognosis for prostate cancer?
a) Prostate cancer prognosis can vary depending on several factors, including the stage and grade of the cancer, the age and overall health of the individual, and the response to treatment. It is important to consult with a healthcare professional for an accurate prognosis based on individual circumstances.
b) Prostate cancer is typically categorised into different stages based on how far the cancer has spread. The most commonly used staging system is the TNM system, which evaluates the tumour size and extent of spread to nearby lymph nodes and other organs. Another important factor is the Gleason score, which indicates the aggressiveness of the cancer based on the appearance of cancer cells under a microscope.
c) In general, localized prostate cancer (confined to the prostate gland) has a favourable prognosis, with high survival rates. The 5-year relative survival rate for localised prostate cancer is nearly 100%. Many men with localised prostate cancer can be effectively treated and experience long-term survival.
d) For locally advanced prostate cancer (spread beyond the prostate but still within the pelvic area), the prognosis can vary. With appropriate treatment, including radiation therapy, hormone therapy, and sometimes surgery, the 5-year relative survival rate is around 70% to 90%.
e) Metastatic prostate cancer (cancer that has spread to distant organs like bones, liver, or lungs) is generally more challenging to treat. The prognosis for metastatic prostate cancer varies widely, depending on the extent of metastasis and the response to treatment. With advancements in treatment options, such as chemotherapy, hormone therapy, targeted therapies, and immunotherapy, the survival rates for metastatic prostate cancer have improved over the years. The 5-year relative survival rate for metastatic prostate cancer is approximately 30% to 35%.
f) It's important to note that these statistics are general and can vary significantly from person to person. Many factors can influence an individual's prognosis, so it's best to consult with a healthcare professional who can provide personalised information based on the specific circumstances of the patient.
Are there any support groups or resources available for prostate cancer patients and their families?
Yes, there are several support groups and resources available for prostate cancer patients and their families in Australia. Here are a few notable ones:
a) Prostate Cancer Foundation of Australia (PCFA): PCFA is a national organisation that provides support, information, and resources for men affected by prostate cancer. They offer a range of services, including support groups, online communities, and educational materials. Their website (https://www.pcfa.org.au/) is a valuable resource for accessing information about prostate cancer, treatment options, and support services.
b) Cancer Council Australia: Cancer Council is a leading cancer organization in Australia that provides support services to cancer patients and their families. They offer various programs, including support groups, counselling services, and online communities. The Cancer Council website (https://www.cancer.org.au/) provides information on prostate cancer, treatment options, and support services available in different states and territories.
c) Prostate Cancer Support Groups: There are numerous local support groups across Australia specifically for prostate cancer patients and their families. These groups offer a supportive environment for sharing experiences, discussing concerns, and accessing information. You can find local support groups through the PCFA website or by contacting your local hospital or cancer center.
d) Andrology Australia: Andrology Australia is a government-funded organization that focuses on male reproductive health. They provide information and resources on various aspects of men's health, including prostate cancer. Their website (https://www.andrologyaustralia.org/) offers educational materials, fact sheets, and resources for patients, families, and healthcare professionals.
e) Australian Prostate Centre: The Australian Prostate Centre is a specialised center dedicated to prostate cancer care, research, and education. They offer support programs, including peer support groups, counselling services, and educational workshops. Their website (https://www.australianprostatecentre.org/) provides information on their services and resources.
f) PROST! exercise 4 Prostate Cancer Inc. (www.prost.com.au) undertakes evidence-based group exercise sessions in 5 locations in Western Australia focusing on Mateship Muscle Mood.
PROST! provides a holistic approach where the whole is greater than the sum of the parts. Muscle being the evidenced-based group exercise sessions. Mateship generated through the experiences and companionship of men going through the prostate cancer journey. And Mood is the sum of the Muscle and Mateship. It assists in overall health and improvement in mental wellbeing.
The three components are what PROST! is all about. Helping men in their fight to overcome the effects of being diagnosed with prostate cancer.
It's important to note that the availability of support groups and resources may vary depending on your location within Australia. It's recommended to visit the mentioned websites or reach out to local healthcare providers to find specific support services in your area.
How often should men get screened for prostate cancer?
The recommended frequency for prostate cancer screening in men depends on various factors and may vary based on different guidelines and individual risk factors. It's essential to consult with a healthcare professional or a urologist to determine the most appropriate screening schedule for an individual. However, here are some general guidelines:
a) Age and Risk Factors: It Is recommended men discuss the potential benefits and risks of prostate cancer screening with their healthcare provider starting at age 50 for average-risk men. For men at higher risk, such as those with a family history of prostate cancer or Australian aboriginal men, the discussion may begin at age 40 to 45.
b) PSA Testing: Prostate-specific antigen (PSA) blood test is commonly used for prostate cancer screening. Depending on the results and individual risk factors, the frequency of PSA testing may vary. Typically, a baseline PSA test is performed, and subsequent testing intervals are determined based on the results and any changes over time.
c) Individualised Approach: Screening intervals can be personalised based on the initial PSA level, rate of change, age, health status, and other risk factors. Some men may require more frequent testing, while others may have longer intervals between screenings.
It's crucial to note that the decision to undergo prostate cancer screening should be made on an individual basis, considering the potential benefits and harms. Screening can lead to early detection and treatment of prostate cancer but may also result in false-positive results, unnecessary biopsies, and overdiagnosis. Ultimately, discussing the potential benefits and risks with a healthcare professional is essential in making an informed decision about screening frequency.
Can prostate cancer spread to other parts of the body?
Yes, prostate cancer can spread to other parts of the body. This process is known as metastasis. Prostate cancer commonly spreads to nearby lymph nodes, bones (such as the spine, pelvis, or hips), liver, lungs, or other distant organs.
The spread of prostate cancer typically occurs through the bloodstream or lymphatic system. Cancer cells can break away from the original tumour in the prostate gland and travel to other areas of the body, where they can form new tumours and continue to grow.
It is important to note that not all prostate cancers spread, and the likelihood of metastasis depends on various factors such as the stage of cancer, the grade of the tumour, and individual characteristics of the patient. Regular screening, early detection, and appropriate treatment can help manage and potentially prevent the spread of prostate cancer.
How does age affect the risk of developing prostate cancer?
Age is a significant risk factor for prostate cancer. The likelihood of developing prostate cancer increases with age, and the majority of cases are diagnosed in older men. Here's how age affects the risk of developing prostate cancer:
a) Increased incidence: The incidence of prostate cancer rises significantly with advancing age. While prostate cancer can occur in younger men, it is primarily a disease of older individuals. The risk increases progressively after the age of 50 and becomes more pronounced after the age of 65.
b) Age-specific prevalence: Studies have shown that prostate cancer is relatively common among men in their 60s and 70s, with the highest incidence rates observed in men aged 70 to 74. By the age of 80, a significant percentage of men may have prostate cancer, even if it is not causing symptoms or affecting their health.
c) Aggressiveness: Age can also influence the aggressiveness of prostate cancer. Older men are more likely to develop aggressive forms of the disease compared to younger men. Aggressive prostate cancer is characterised by a higher likelihood of spreading beyond the prostate gland and may require more aggressive treatment approaches.
d) Screening recommendations: Due to the increased risk associated with age, various medical organisations recommend prostate cancer screening for men based on their age and individual risk factors. Screening typically involves a prostate-specific antigen (PSA) blood test and, if necessary, a digital rectal exam (DRE). The frequency and initiation of screening may vary based on guidelines and individual patient factors.
It's important to note that age is just one factor contributing to the risk of developing prostate cancer. Other factors, such as family history, race, and lifestyle choices, can also influence the likelihood of developing the disease. Regular check-ups with a healthcare provider and discussions about personalised screening strategies can help men make informed decisions about their prostate health based on their age and individual risk factors.
What is the Gleason Score in Prostate Cancer?
The Gleason score is a system used to grade prostate cancer based on the microscopic appearance of cancer cells in a prostate tissue sample. It helps provide important information about the aggressiveness and potential behaviour of the cancer. Here are some key points about the Gleason score:
Scoring system: The Gleason score is determined by evaluating the patterns of cancer cells under a microscope. The pathologist assigns a primary and secondary pattern, each graded on a scale from 1 to 5. The two grades are added together to create the Gleason score, which typically ranges from 6 to 10.
Gleason patterns: The primary pattern represents the most predominant cancer cell pattern observed, while the secondary pattern reflects the second most common pattern. The patterns describe how cancer cells are arranged and their resemblance to normal prostate tissue.
Grade groups: To simplify interpretation and clinical decision-making, the Gleason score is often grouped into five categories called Grade Groups. Grade Group 1 corresponds to a Gleason score of 6, which is considered low-grade. Grade Group 5 corresponds to a Gleason score of 9 or 10, indicating a high-grade cancer.
Prognostic significance: The Gleason score is an essential factor in determining the aggressiveness and potential outcomes of prostate cancer. Higher Gleason scores are generally associated with a more aggressive cancer that is more likely to grow, spread, and require more aggressive treatment.
Treatment implications: The Gleason score is a crucial consideration when deciding on the appropriate treatment strategy for prostate cancer. It helps guide decisions such as active surveillance, surgery (prostatectomy), radiation therapy, hormone therapy, or other treatments.
Can my diet reduce the incidence of prostate cancer?
Diet can play a role in reducing the risk of prostate cancer, although it's important to note that no single factor can guarantee prevention. However, maintaining a healthy diet can contribute to overall well-being and potentially lower the risk of various diseases, including prostate cancer. Here are some dietary considerations that may help reduce the incidence of prostate cancer:
Eat a balanced diet: Consume a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. A well-rounded diet ensures you receive essential nutrients, vitamins, and minerals that support overall health.
Increase plant-based foods: Include a significant portion of plant-based foods in your diet. Fruits, vegetables, legumes, and whole grains are rich in antioxidants, phytochemicals, and fiber, which may have protective effects against prostate cancer.
Choose healthy fats: Opt for healthy fats such as those found in olive oil, avocados, nuts, and seeds. These fats provide beneficial omega-3 fatty acids and may help reduce inflammation in the body.
Limit red and processed meats: High consumption of red and processed meats has been associated with an increased risk of prostate cancer. Try to reduce your intake of beef, pork, lamb, and processed meats like hot dogs and sausages.
Opt for lean protein sources: Include lean protein sources in your diet, such as poultry, fish, tofu, beans, and legumes. These options provide essential nutrients while being lower in saturated fat compared to red meats.
Increase fish consumption: Fatty fish like salmon, sardines, and trout are excellent sources of omega-3 fatty acids. These healthy fats may have a protective effect against prostate cancer.
Consume soy products: Incorporate moderate amounts of soy products like tofu, edamame, and soy milk into your diet. Soy contains compounds called isoflavones, which may have protective effects against prostate cancer.
Stay hydrated: Drink an adequate amount of water throughout the day. Staying hydrated supports overall health and helps maintain proper bodily functions.
Maintain a healthy weight: Obesity has been linked to an increased risk of prostate cancer. By following a balanced diet and engaging in regular physical activity, you can maintain a healthy weight and reduce your risk.
Remember that dietary factors are just one aspect of prostate cancer prevention. It's also essential to lead a healthy lifestyle, exercise regularly, avoid tobacco products, limit alcohol consumption, and undergo regular check-ups with your healthcare provider. They can provide personalised advice based on your individual health status and risk factors.